Secondary lymphedema results from an identifiable damage leading to disruption or obstruction of normally functioning lymph vessels and/or lymph nodes and may present in the extremities, trunk, abdomen, head and neck and external genitalia.
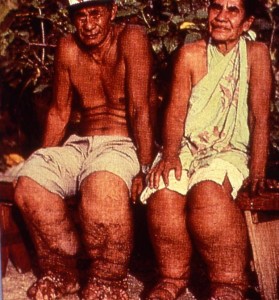 Worldwide, the most widespread cause of secondary lymphedema is an infection with a thread-like worm named wucheria bancrofti, which leads to a condition known as filariasis. This is a tropical disease, endemic in more than 80 countries in Africa, India, Southeast Asia, and South America, as well as in the Pacific Islands and the Caribbean. According to the World Health Organization, 1.3 billion individuals are threatened by the disease and over 120 million people are currently affected by it, with about 40 million individuals being disfigured by lymphedema and suffering from recurrent infections and other secondary conditions.
Worldwide, the most widespread cause of secondary lymphedema is an infection with a thread-like worm named wucheria bancrofti, which leads to a condition known as filariasis. This is a tropical disease, endemic in more than 80 countries in Africa, India, Southeast Asia, and South America, as well as in the Pacific Islands and the Caribbean. According to the World Health Organization, 1.3 billion individuals are threatened by the disease and over 120 million people are currently affected by it, with about 40 million individuals being disfigured by lymphedema and suffering from recurrent infections and other secondary conditions.
Research indicates that the factors causing lymphedema are not solely attributed to lymph and fluid accumulation in the interstitial tissue. It is proposed that its pathophysiology also involves different tissue compartments (excess deposits of adipose tissue in subcutaneous and muscle tissue; fibrotic tissue affecting the skin, the subcutaneous tissues, as well as the walls of lymph collectors, which further impairs their function; thickening/hardening of the skin with possible additional skin changes, such as warts, papillomas, ulcerations and in rare cases cutaneous angiosarcoma) (7).
The highest incidence of secondary lymphedema in the United States is observed following surgery and radiation for malignancies, particularly among those individuals affected by breast cancer.
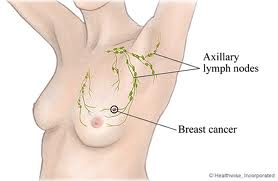 Other than skin cancer, breast cancer is the most common type of malignancy among women in the United States. All women are at risk for developing breast cancer; males are also affected at a ratio of one male to 100 females (1). With increasing age, the greater a woman’s chance of developing breast cancer with the majority of breast cancer cases occurring in women over 50 years of age. While breast cancer is less common at a young age (e.g., women in their thirties), younger women tend to have more aggressive breast cancers than older women, which may explain why survival rates are lower among younger women. Incidence also varies within ethnic groups and geographical location within the U.S.
Other than skin cancer, breast cancer is the most common type of malignancy among women in the United States. All women are at risk for developing breast cancer; males are also affected at a ratio of one male to 100 females (1). With increasing age, the greater a woman’s chance of developing breast cancer with the majority of breast cancer cases occurring in women over 50 years of age. While breast cancer is less common at a young age (e.g., women in their thirties), younger women tend to have more aggressive breast cancers than older women, which may explain why survival rates are lower among younger women. Incidence also varies within ethnic groups and geographical location within the U.S.
Generally, it can be said that one out of eight women in the U.S. will develop breast cancer during the course of their lives. Over 281,000 new cases of invasive breast cancer (over 49,000 non-invasive) in females and 2600 in males are estimated in the United States in 2021 (2). Secondary lymphedema is becoming more common, due to increasing cancer rates, affecting 1 in 1,000 persons, whereby 24–49% of cancer patients develop secondary lymphedema after receiving cancer treatment (7). However, the rate of incidence is likely underestimated because lymphedema remains under-recognized and under-documented to this day.
Why does lymphedema develop?
 Any type of surgery, specifically procedures that require the removal of lymph nodes, can cause the onset of lymphedema. Surgical procedures in cancer therapy, such as breast conserving (lumpectomy) or more extensive breast surgery (mastectomy) commonly include the removal (dissection) of lymph nodes, with subsequent damage to lymph vessels.
Any type of surgery, specifically procedures that require the removal of lymph nodes, can cause the onset of lymphedema. Surgical procedures in cancer therapy, such as breast conserving (lumpectomy) or more extensive breast surgery (mastectomy) commonly include the removal (dissection) of lymph nodes, with subsequent damage to lymph vessels.
Many individuals receive radiation therapy following the surgical procedure, which may aggravate the situation.
The goal of these procedures is to eliminate the cancer cells and to save the patient’s life. A side effect in lymph node removal is the disruption in the transport of lymphatic fluid.
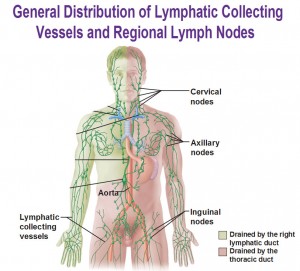
The lymphatic system consists of lymph vessels and lymph nodes throughout the body. Lymph vessels collect lymphatic fluid, which is composed of protein, water, fats, and waste products from cells. These vessels transport the fluid to the lymph nodes, where waste products and foreign materials are filtered out from the fluid. After passing several groups of lymph nodes, the lymph vessels return the fluid back to the blood.
 When the vessels are damaged, the flow of lymphatic fluid is compromised. If the remaining lymph vessels that are unaffected by the surgery are not able to compensate for the damaged vessels, lymphatic fluid accumulates in the tissues. This accumulation of lymphatic fluid results in abnormal swelling, most commonly affecting the upper and lower extremities; however, other parts of the body may be affected as well.
When the vessels are damaged, the flow of lymphatic fluid is compromised. If the remaining lymph vessels that are unaffected by the surgery are not able to compensate for the damaged vessels, lymphatic fluid accumulates in the tissues. This accumulation of lymphatic fluid results in abnormal swelling, most commonly affecting the upper and lower extremities; however, other parts of the body may be affected as well.
Other surgeries, to include treatment of melanoma, cancer affecting the genitourinary and gynecologic systems, cancers in the head and neck region, or soft tissue malignancies, generally include the removal of lymph nodes with subsequent disruption of lymphatic pathways, which may cause the onset of lymphedema.
 Radiation therapy, specifically if combined with the surgical removal of lymph nodes, can cause scarring in soft tissue and inflammation of lymph nodes and lymph vessels, which may also contribute to the development of secondary lymphedema.
Radiation therapy, specifically if combined with the surgical removal of lymph nodes, can cause scarring in soft tissue and inflammation of lymph nodes and lymph vessels, which may also contribute to the development of secondary lymphedema.
Less common causes for secondary lymphedema include surgeries other than for the treatment of malignancies, or trauma disrupting the flow of lymph. Tumors growing in the soft tissues can become large enough to cause a physical block on lymphatic structures subsequently obstructing the normal flow of lymph.
Secondary cases of lymphedema may occur immediately following the surgical procedure and/or radiation, within a few months, a couple of years, or twenty years or more after treatment. The average time of onset is between 14 and 24 months post-surgically, with an increased number of cases over time. Some individuals may never experience any symptoms; however, the risk of development of secondary lymphedema lasts a lifetime.
There is no consistency in the data on the incidence of lymphedema, and most statistics that are available are those on breast cancer related lymphedema (BCRL) affecting the upper extremities.
It was reported that the five-year cumulative incidence of lymphedema following breast cancer surgery in women was 42%; of the affected women, 80% developed lymphedema within two years and 89% within three years (3). A study, which was published in 2001 (conducted by Petrek et al), followed 263 patients after mastectomy and complete axillary dissection. At 20 years after treatment, 49% reported lymphedema; of those, 77% noted onset within three years after surgery, and the remaining women developed lymphedema in the arm at a rate of almost 1% per year (4).
Click here for a short video on the incidence of secondary lymphedema
Prevention
Patient education about the possibility of developing secondary lymphedema, discussion of the risk factors and risk reduction practices, combined with appropriate surveillance and prompt reporting of symptoms following cancer treatment, can limit the incidence and progression of secondary lymphedema.
A recent study (5) including patients who received treatment for breast cancer, determined that patients who received information about the possible onset of secondary lymphedema demonstrated significantly reduced symptoms when compared with patients who did not receive this information. Women who received information about lymphedema were significantly less likely to report heaviness in the extremity, arm swelling, impaired shoulder mobility, and breast swelling.
The NLN’s position statement on risk reduction practices (6) serves as a valuable resource.
Early treatment of secondary lymphedema by a qualified therapist is of paramount importance to limit progression of the swelling and to avoid complications often associated with untreated or incorrectly treated lymphedema.
The treatment of choice for this condition is complete decongestive therapy (CDT), a combination of modalities including manual lymphatic drainage, the application of padded short-stretch bandages, use of compression garments, therapeutic exercise, and skin care.
Click here for a short video on the importance of treatment
Dear Lymphedema Blog Reader – if you like the contents on this website, please help to keep it going. A great amount of work and research is necessary to provide you with up-to-date information on this site. Your donation supports these efforts and associated administrative costs. Surplus funds will be donated to Lymphedema/Lipedema-related charitable endeavors. Please donate using the “Donate Now” button on the right upper hand of this page – Thank You!
Join Lymphedema Guru, a Facebook page solely dedicated to inform about all things related to lymphedema – news, support groups, treatment centers, and much more
1.http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-029771.pdf
2. https://www.breastcancer.org/symptoms/understand_bc/statistics
3. http://cebp.aacrjournals.org/content/19/11/2734.long
6. https://issuu.com/lymphnet/docs/risk_reduction
7. https://www.frontiersin.org/articles/10.3389/fphys.2020.00137/full

 Joachim Zuther, Lymphedema Specialist.
Joachim Zuther, Lymphedema Specialist. 

Every time I read your most informative blog, it reminds me: what ever happened to the legislation that was in the works about two years ago, to pay for the various oppressive costs that accompany recommended therapies for lymphedema? How many persons can get the benefits of lymphedema therapists when no reimbursement is possible?
Just wondering . . .
Thank you for your writings.
Dear George: For any up-to-date information, please go to http://lymphedematreatmentact.org/
Thank you very much for your dedication to informing us all and assisting our patient care skills. Your book has been a continuous source of information and inspiration for several years.
Can you do some writing on the post surgical secondary edema from lymph vessel disruption from routine orthopedic incision and resultant scar (e.g., posterior total hip approach) and from abdominal incisions?
These days it seems I am constantly refocusing care towards scar tissue mobility and lymph drainage (decongestive therapy) after injury and surgery.
Your thoughts would be welcomed.
Dear Jonathan: Absolutely, I will work on a post covering this issue in the future. Depending on the extent and the quality of the scar, it can pose a significant blockage of normal lymphatic flow. MLD is important in the early post-operative stage in order to decongest the area surrounding the scar. The focus is to improve oxygenation and nutrition in this area by removing stagnant fluid, thereby decresing diffusion distance between the blood capillaries and the affected tissues. Scar tissue tends to heal faster and the chance of adhesions and keloids is significantly reduced as well.
I have had lymphedema in both legs from the knees down for 11 years. It is very inconsistent even though I have had manual lymph drainage at a hospital.
My insurance is Medicare Advantage. Once I had received all the denials from my doctor and my insurance: Medicare was responsible. I went before an administrative judge: at first she denied treatment. I went to another vascular surgeon and received treatment.
Then I went before a Medicare judge, and with the help of a wonderful lymphedema volunteer I received hose (custom made or not) from my insurance company with only 20% co-pay.
You just have to keep advocating for yourself!! (And finding help.)
Hi Neva,
Good to hear that you are still in there advocating. Your case was the third case I argued before the Medicare Appeals Council in Washington.
I’m still providing help in insurance and Medicare appeals to those wishing to fight the good fight.
LymphActivist@aol.com
Your blogs are very interesting but still cannot answer my problem. As fas my Lymphodema, I have had no surgeries, no treatment for cancer or anything I have seen in your blogs. I am a type 2 diabetic, and obese. My Lymphodema started about 15 years ago when I was first informed I was a diabetic and the the doctor gave a pill called avandia to keep my blood sugars under control, well it did something else and made my retain fluid and have had this problem ever since. I am now on insulin, with a different doctor but still cant seem to beat my Lymphodema. Any and all help would be appreciated.
Dear Marcial: The swelling you are experiencing may be edema and not lymphedema. I would like to refer you to two articles that may be helpful to you to find out more.
1. http://www.lymphedemapeople.com/thesite/lymphedema_and_diabetes.htm
2. https://www.lymphedemablog.com/2011/06/23/when-is-it-lymphedema/
[…] statistics vary greatly but in a blog post from Jo Zuther, founder of the Academy of Lymphatic Studies, There is no consistency in the data […]
[…] Primary Lymphedema and Secondary Lymphedema usually progress through a series of stages. That’s why it’s important to get help right away, […]
I have Lymphedema in my lower extremities & have read that there are 2 stages that are reversable. Can you tell me how that is done. I went undiagnosed for 3 years & had PT twice in 1 year. Lucky for me the hospital closed their PT centers. I’m with a therapist now that specializes in Lymphedema & wow what a difference! She has taught me so much about the disease & how to do my own self Lymph massage. Sadly No one can tell me why I have Lymphedema but I had all the signs. I kept a list of all the things that were on going but not one doctor I went to, & there were 4, picked up on it until I went to a vein clinic as I was concerned that I had a blood clot or deep vein thrombosis. The second the nurse saw my legs she said, oh my gosh, you have Lymphedema!! I’ve had many abdominal surgeries & have also had my esophagus removed. I still have no diffitive answers but I’m beginning to think my Lymphatic Systems has been damaged at some point. Can you help? Any ideas, suggestions or articles that may give me some answers would be greatly appreciated.
Mollie: Lymphedema is treated with complete decongestive therapy (CDT). Here is a link explaining the therapy: https://www.lymphedemablog.com/2012/07/03/complete-decongestive-therapy-in-the-treatment-of-lymphedema/
Please click on the “Find a Therapist” link on the menu bar on top of this page to locate a certified therapist in your area.
I’m interested in this article you fail to mention Lipoedema (Lipedema) as a cause for secondary lymphoedema. Lymphoedema is a significant issue in Stage 3 and 4 lipoedema . Anyone who is clasified as “obese” and is unable to lose weight from the lower half of the body may have this, as I do. I was originally diagnosed as lymphoedema but now know I only have a small amount of lymphoedema as a result of my Lipoedema.
Lymphoedema Conferences around the world are now addressing this issue..eg Asia Pacific Lymphology Conference in Darwin Australia in May 2016.
Thank you for your valuable input, Elizabeth. Here is a link to an article addressing this topic: https://www.lymphedemablog.com/2012/12/13/a-closer-look-at-lipedema-and-the-effects-on-the-lymphatic-system/
Are you aware of any clinical trials that are working on a cure for secondary lymphoedema?
No, I am not.
I have severe lymphedema in my right leg following my last pregnancy 9 yrs ago. No one can tell me why I got it . I had skinny leg before that lympocentography showed absent lymph nodes but how do I suddenly loose my lymph nodes. I was interested to know if the worm could have caused it .how would I know and if so if it is treated can the lymphedema be reversed. I have tried all treatment including alternative therapies and one therapist said it is a psychological blockage can this be true I will try anything I feel so unwell fatigued and brain fogged short of breath and lower self esteem as its very difficult to get trousers and shoes to fit as my left side is normal thank god.any advice would be great.
Mary, your symptoms and history point toward primary lymphedema. I would suggest seeking consultation with a certified lymphedema therapist. You can locate a therapist in your area by using the link “Find a Therapist” in the menu bar at the top of this page.