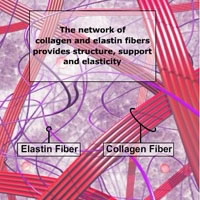
 It is important to understand that the elastic fibers in the tissues affected by lymphedema are damaged. These fibers lose their elasticity and tend to harden, which is particularly the case in untreated lymphedema present over a long period of time and progressed stages of lymphedema.
It is important to understand that the elastic fibers in the tissues affected by lymphedema are damaged. These fibers lose their elasticity and tend to harden, which is particularly the case in untreated lymphedema present over a long period of time and progressed stages of lymphedema.
Although the swelling in lymphedema may be reduced to a normal or near normal size during treatments, the damage to the lymphatic system, which caused the onset of lymphedema, is permanent and the skin elasticity in the tissues affected by lymphedema may never be regained to prior levels.
Contrary to edema, a low-protein swelling, lymphedema is a disease rather than a symptom and its underlying cause, the insufficiency of parts of the lymphatic system cannot be reversed.
 Lymphedema results from the inability of the lymphatic system to perform one of its basic functions, the removal of water and protein from the tissues of a portion of the body. This insufficiency can be caused by developmental abnormalities of the lymphatic system (primary lymphedema), or damage to the lymphatic system such as the removal or radiation of lymph nodes in cancer surgery, or infection of the lymphatic system (secondary lymphedema).
Lymphedema results from the inability of the lymphatic system to perform one of its basic functions, the removal of water and protein from the tissues of a portion of the body. This insufficiency can be caused by developmental abnormalities of the lymphatic system (primary lymphedema), or damage to the lymphatic system such as the removal or radiation of lymph nodes in cancer surgery, or infection of the lymphatic system (secondary lymphedema).
The accumulation of protein and water in the tissues may be gradual in some patients and sudden in others, the result is always a high-protein edema.
Lymphedema does not dissipate by itself and continues to progress without adequate treatment.
The goal of lymphedema management is to reduce the lymphedematous swelling to a normal or near normal size utilizing remaining healthy lymph vessels and other lymphatic pathways. Once the lymphedema is decongested, the secondary goal is to maintain the reduction and to prevent the re-accumulation of lymph fluid.
These goals can be achieved with the internationally recognized “gold standard” of lymphedema treatment known as Complete (or Combined) Decongestive Therapy (CDT). CDT is a combination of the following treatment modalities:
Manual lymph drainage (MLD), skin care, decongestive exercises and compression therapy.
 Compression therapy in lymphedema management is provided either via bandages, compression garments or alternative compression devices (depending on the stage of treatment).
Compression therapy in lymphedema management is provided either via bandages, compression garments or alternative compression devices (depending on the stage of treatment).
Compression bandages and garments by themselves will not reduce existing swelling and must therefore not be worn on an untreated, swollen extremity.
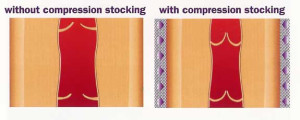
 Individuals affected by lymphedema graduate from padded short-stretch bandages, which are applied by the lymphedema therapist in the intensive phase of CDT to elastic compression garments only when the affected extremity is decongested. To assist in the movement of fluids back to the heart, a pressure gradient between the lower (higher pressure) and the upper part (lower pressure) of the extremity is provided with bandages and garments.
Individuals affected by lymphedema graduate from padded short-stretch bandages, which are applied by the lymphedema therapist in the intensive phase of CDT to elastic compression garments only when the affected extremity is decongested. To assist in the movement of fluids back to the heart, a pressure gradient between the lower (higher pressure) and the upper part (lower pressure) of the extremity is provided with bandages and garments.
Even after successful treatment, the body part affected by lymphedema is at permanent risk for re-accumulation of fluid and most individuals affected by lymphedema are aware of the fact that this condition requires life-long care.
Without the benefits of external compression successful long-term management of lymphedema would be very difficult and in most cases impossible.
So why is compression therapy an essential component in lymphedema management?
As explained, the elastic fibers in lymphedema are damaged and thus unable to provide sufficient resistance to the build-up of fluid in the interstitial tissue spaces. The application of external compression provides the necessary support for those tissues that lost elasticity and compensates for the elastic insufficiency by increasing the tissue pressure.
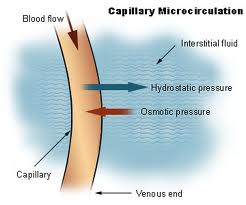 The tissue pressure plays an essential role in the exchange of fluids between the blood capillaries and the tissue. The increased tissue pressure provided by external compression reduces the amount of fluid leaving the blood capillaries into the tissues and increases the return of tissue fluids back into the blood and lymph capillaries, thus reducing the amount of fluid in the tissues.
The tissue pressure plays an essential role in the exchange of fluids between the blood capillaries and the tissue. The increased tissue pressure provided by external compression reduces the amount of fluid leaving the blood capillaries into the tissues and increases the return of tissue fluids back into the blood and lymph capillaries, thus reducing the amount of fluid in the tissues.
 External compression also increases venous and lymphatic return by improving the function of the valves in these vessels. Another important factor for sufficient return of venous and lymphatic fluids back into the blood stream is the movement of skeletal musculature and joints during activity. Together with other supporting mechanisms the muscle and joint pump activity propels these fluids back to the heart and ensures uninterrupted circulation.
External compression also increases venous and lymphatic return by improving the function of the valves in these vessels. Another important factor for sufficient return of venous and lymphatic fluids back into the blood stream is the movement of skeletal musculature and joints during activity. Together with other supporting mechanisms the muscle and joint pump activity propels these fluids back to the heart and ensures uninterrupted circulation.
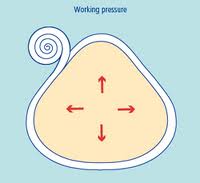 External compression provides a counter force to the working musculature, known as working pressure, thus improving its efficiency.
External compression provides a counter force to the working musculature, known as working pressure, thus improving its efficiency.
These effects help to prevent re-accumulation of fluids which were evacuated during intensive CDT treatments and conserve the results achieved during MLD.
Another positive impact of compression therapy is the softening of hardened connective tissue often present in lymphedema, especially if external compression therapy is combined with special foam materials.
More articles on this subject:
How to Care for Compression Garments
Click here for a PDF Version of this Article
Dear Lymphedema Blog Reader – if you like the contents on this website, please help to keep it going. A great amount of work and research is necessary to provide you with up-to-date information on this site. Your donation supports these efforts and associated administrative costs. Surplus funds will be donated to Lymphedema/Lipedema-related charitable endeavors. Please donate using the “Donate Now” button on the right upper hand of this page – Thank You!
Join Lymphedema Guru, a Facebook page solely dedicated to inform about all things related to lymphedema – news, support groups, treatment centers, and much more

 Joachim Zuther, Lymphedema Specialist.
Joachim Zuther, Lymphedema Specialist. 

I had six weeks of treatment for lymph edema. Also was diagnosed with multiple myeloma. My legs were worse after treatment. They hurt all the time. I wore compression bandages at night, but don’t do it any longer. I wear compression hose every day. Can’t understand why my legs were worse after therapy.
I have a Lymph edema air compression pump now for my legs and it has been keeping swelling down in my legs. What are your thoughts on the pump?
I have a Lymphapress machine, made in Israel. The protocol ten plus years ago was to always use maximum pressure (50mm Hg) for a minimum of 2 hours at each session. I followed that, and did 2 sessions each day(about 5 hours total.) IT WAS A DISASTER! I turned my leg rock hard and was then subject to cellulitis a number of times.
A much lower pressure, in fact the lowest possible, would be my advise. I will return to the pump, and will use a very low pressure setting.
Also one therapist I was very fortunate to have treatments from (she was trained in Venezuela) taught me to use Lycra stockings, not the 40-50 # heavy duty stockings. I am MUCH more comfortable, and because I can stand the feeling, I wear them much more often and therefore have better control.
I have no experience with the pump. I wear 20/30 compression hose. They help but my legs still hurt.
[…] image taken from: https://www.lymphedemablog.com/2014/12/05/the-science-behind-compression-therapy-in-lymphedema-manage… […]
I too have a lymphapress pump. I have tried hi and low numbers. on low 39 my arm still swells after I pump. it has never reduced my swelling only increased it.is this normal?
Dear Joan – unfortunately I am unaware of proper settings on these devices. We do not support the use of compression pumps without accompanying complete decongestive therapy
Interesting read on the benefits of compression garments in supporting lymphedema recovery
I have a FloTron machine for my legs, which is a pressure treatment sleeve system that I use for my legs but I’m finding it very hard…my legs are swelling more each day & are becoming more solid. I have a genetic form of Lymphedema, which went undiagnosed for 17 years.
URGENTLY NEED HELP PLEASE!!!
I live in Finland and LE therapy is not good in my smaller city. After my dominant side mastectomy in August the hospital physical therapist instructs all patients post-op to do range of motion exercises immediately. I didn’t know I had had 9 nodes removes until the final path was ready three weeks post-op, had thought it was just sentinal nodes. My BC is very aggressive and HER 2 + but the nodes were all clean.
The PT told me to treat my severe cording (nurse said worse she’d ever seen) by increasing ROM exercises and forcing my arm up by leaning against a wall. I know now that was so wrong. Pain then swelling from LE began within a week, dg made 29.9. And she just gave me an OTC Jobst sleeve, a poorly fitting Lymed glove (said sew it tighter yourself), nothing for my chest wall LE.
My husband’s rehab doctor friend recommended a private LE therapist trained in the Vodder method. The first visit she wrapped but I hardly remember anything because my brain was so foggy from second dose of chemo the week before. The bad-fitting glove broke the skin between my thumb and first finger, so I used nothing for three days. Then I woke up with my hand so swollen and sore I couldn’t even make a half fist, not even around a coffee mug. Did elevation over shoulder level for four hours and got it down enough to use, but never to the same glove size.
That LE therapist saw me again last Weds., did some kind of decongestive massage, and wrapped me again. I’ve been reading the materials she gave me and also on the wonderful community.breastcancer.org site and understand a bit more. I have been frustrated trying to wrap but succeeded in sleeping the pat two nights wrapped. When I remove the wrap and use the sleeve and glove, the LE worsens.
MY URGENT PROBLEM: HOW DO I HANDLE COMPRESSION DURING CHEMO INFUSIONS?
I get chemo again in 4 days, and the high dose Dexamethasone the night before and twice chemo day causes water retention (about 3kg). I already have finrgertip numbness — neuropathy from the Taxotere — that I am afraid might worsen if I stuff myself into the sleeve/glove during the infusion (slow blood flow, cause more neuropathy?) Wrapping would make cold glove use impossible (only got right hand for my last — 2. –dose and it seems to have lessened the worsening on that side; I’d like to cold glove again. My LE therapist said to just leave everything off the swelling will maybe go down again. But I am afraid of permanently ripping the tissue. I already went through that swelling crisis when I stopped all compression and am frightened of that happeneing again, and leaving my hand even more swollen. My left hand/arm are hampered by longterm nerve damage a neck operationdid not help, and now also by the numbness (neuropathy) so I need to save my right hand function.
Does LE always rebound when you stop compression?
I was considering keeping wrapped now 23/7 then all off for the several hours of infusion to try to remove as much LE as possible — but just read here that that will NOT work, one needs the massage which I only had once and will get again Tues I think.
I would be extremely grateful for any help/advice you could give me ASAP.
Thank you. I am near to losing hope.
Dear Leslie: Lymphedema does not always rebound without compression, but it generally does. The most effective way to control and manage lymphedema is to go through a proper treatment sequence with complete decongestive therapy, which should be applied on a daily basis until the swelling is down to a normal or near normal size. I am unable to give you any advice on how to handle your swelling while going through chemotherapy, however a good lymphedema therapist, who knows your personal situation, should certainly be bale to give you sound and meaningful advice on the necessary steps.
Thank you.
I have lymphedema in my torso and arms which came after bilateral implants were removed 10 years after placement. The tissue was black so the surgeon removed all scaring. Since 2013, I’ve had several series with lymph therapists. I also wear compression sleeves and swim and do self MLD about 5 times per week after swimming. I can’t find a compression garment for my torso because my underarms continue to get bigger and the one that I was fitted for was sleeveless. My therapist strongly encouraged me to talk with a surgeon who does microsurgical procedures. I would go through that if it would improve my long term outcome but now I feel the tissue in my upper arms is hardening and wonder what will happen to my torso? None of my therapists suggest any garments for it and I can’t find a fitter to measure me for a garment. I would appreciate any suggestions. I try to manage this but the pain sometimes is overwhelming. Thanks.
Without knowing you personally, I am unable to make any specific recommendations, but would highly advise to seek appropriate compression for the areas affected by swelling. Tissues tend to become fibrotic if the swelling is not kept under control.
I have had different answers from therapists and doctors regarding the use of kinesiotape under compression garments and bandages. Opinions include: 1)the more compression methods the better, 2)only one form of compression is effective at a time, 3) tape and other methods work against each other, and 4)it makes no difference whatsoever what combination is used. All the forms of compression are effective for me individually. I am also interested in the effective life of the kinesiotape. Again, answers vary from it’s good for 24 hours to it being effective as long as it’s on. I am concerned about using my compression effectively and taking off tape at the optimal times to avoid skin damage. Thanks!!!!
Hi,
I have been receiving MLD with Multi-layered Compression Bandaging now for almost 9 years. I have a Primary that was not picked up on and also a secondary following a car crash. My story is a long one however I am wondering if you could possibly give me some advice.
I am trying to wear compression bandagings less on my full legs and manage in support tights more the problem is I still experience rather bad refill and further more I have a lot of scars representing previous surgeries following large weight loss (over 500 lbs) and the support tights are painful on my extensive scars!!! 😔 I was interested if you could please offer any suggestions and light on my life long situation.
I also have areas of stubborn fibrosis of the skin and take long term antibiotics due to a history of frequently retuning infection, namely Celulitise 😔
I look forward to your reply.
King Regards in the Best of Health 😇
Valerie ROGERS. 😃
Valerie: You may want to try compression alternatives, which would give you the additional option of padding. Here is a link showing some of these products: http://www.lymphedemastore.com/compression-alternatives/